Just when I think we are on some kind of a level field, the bottom falls out.
There is only one thing that could have been worse than what I have lived in the last year, that would have been receiving word that Pat had been killed in combat.
I am posting this on the blog – so I need to elaborate a little. There are people who read the blog that do not receive the e-mails that contain more information than what has been posted here previously in the last 2-3 months.
For a year, Pat has lived with a bullet in his leg, one of the two gunshot wounds he suffered on September 19, 2008. In late August THIS YEAR, the gunshot wound started showing signs of infection – swelling, redness, warm to the touch. He was taken to a doctor, the gunshot wound was lanced, and blood spewed out of it. Lab work was done which showed an infection. He was eventually put on antibiotics. An additional lab test was done – at my request – it was to evaluate the lead level in his blood. That test result came back as elevated – confirmed on repeat testing.
Nye County Nevada said they would make certain Pat got treated – but that ultimately I would have to pay the bill for the treatment. After much discussion between a Senator’s office, the VA, the District Attorney’s Office and the Sheriff’s Department – it was agreed that the VA would see Pat and that the Sheriff’s Department would transport Pat to the VA for treatment.
That was until Thursday afternoon, when the VA squarely SLAMMED the door in Pat Lamourex’s face once again.
Today is Saturday, October 10, 2009. The bullet remains in Pat’s leg. The gunshot wound is still seeping, so much that it runs down his leg. He has developed an anomaly on both of his arms, which resembles something that occurs when someone is taking blood thinners. It is hard to describe – it resembles bruising, but it is a pooling of blood just under the skin that is not the result of trauma. It just appears.
I called the detention facility Thursday after being told the VA was not going to take care of Pat. I asked them to please have my husband call me – it was important that I speak to him. They refused to relay the message.
It was not until late Friday that Pat finally called, and I gave him the news that we were back at square one. I told him to put in another request for medical treatment. It will be a second opinion; I told him to request repeat lab work, as well as additional lab work that has not been done previously.
There are many possibilities as to what could be causing these “bruising” spots on his arms.
I know that Pat is extremely stressed, and so am I; and he is not getting the appropriate medical treatment from ANYONE for ANYTHING.
This is how we say “Thank you for your service.”
Sue Lamoureux's blog for her husband, J Patrick Lamoureux. Sue died on 24 August 2015.
PAT LAMOUREUX

PAT LAMOUREUX - One episode in a person's life, does not define the person.
Saturday, October 10, 2009
Wednesday, October 7, 2009
PTSD: An Army colonel’s quest for answers
By Kelly Kennedy - Staff writer - Army Times
Posted : Wednesday Oct 7, 2009 14:51:58 EDT
Army Col. Rich O’Connor does not mince words when he talks about the amount of mental health training he had before he took a squadron in the 3rd Armored Cavalry Regiment to war in Iraq’s Diyalah province in 2006.
“What kind of training did I receive on post-traumatic stress?” he said. “Zero. How much did our soldiers receive? None.”
O’Connor told a room of high-ranking officers and enlisted soldiers at the annual Association of the U.S. Army convention that he was too busy training for war to even think about post-traumatic stress disorder. And he said that after talking to other battalion commanders and command sergeants major, he realized nobody else had, either.
Then a military psychiatrist told him she didn’t believe commanders cared about PTSD.
“I can tell you that’s probably true,” O’Connor said. “We’ve got an issue here.”
(Click here for complete story)
http://www.armytimes.com/news/2009/10/military_ausa_ptsd_100709w/
Posted : Wednesday Oct 7, 2009 14:51:58 EDT
Army Col. Rich O’Connor does not mince words when he talks about the amount of mental health training he had before he took a squadron in the 3rd Armored Cavalry Regiment to war in Iraq’s Diyalah province in 2006.
“What kind of training did I receive on post-traumatic stress?” he said. “Zero. How much did our soldiers receive? None.”
O’Connor told a room of high-ranking officers and enlisted soldiers at the annual Association of the U.S. Army convention that he was too busy training for war to even think about post-traumatic stress disorder. And he said that after talking to other battalion commanders and command sergeants major, he realized nobody else had, either.
Then a military psychiatrist told him she didn’t believe commanders cared about PTSD.
“I can tell you that’s probably true,” O’Connor said. “We’ve got an issue here.”
(Click here for complete story)
http://www.armytimes.com/news/2009/10/military_ausa_ptsd_100709w/
Veteran in an Acute Dissociative State
(Acknowledgments: The author would like to thank Alan Maiers, PsyD, Brenda Mayne PhD, and Thea Schneider, CNS, for their helpful review of the article. Dr Geppert is associate professor of psychiatry and director of ethics education at the New Mexico School of Medicine in Albuquerque. She is also chief of consultation psychiatry and ethics at the New Mexico Veterans Affairs Health Care System in Albuquerque. Alan Maiers, PsyD, assistant chief of the COPE Division at the Warrior Resiliency Program in San Antonio, Tex, coauthored the case vignettes that appear in this article. ) Cynthia M. A. Geppert, MD, PhD
October 6, 2009
Psychiatric Times. Vol. 26 No. 10
CASE VIGNETTE
A 24-year-old veteran of Operation Iraqi Freedom (OIF) presents to the ED mid-morning on a weekday. While the veteran is waiting to be triaged, other patients alert staff that he appears to be talking to himself and pacing around the waiting room. A nurse tries to escort the veteran to an ED examination room. Multiple attempts by the ED staff and hospital police—several of whom are themselves OIF veterans—are unsuccessful in calming the patient or persuading him to enter a room.
The increased attention escalates the patient’s behavior and he begins to run around the ED. At one point he hides under instrument trays, yelling out “Incoming! We have to get them before they get us! The enemy is coming for us!” He then runs to another location, as if taking fire.
A quick general status evaluation shows a young man with several days’ growth of beard in jeans and T-shirt who looks sleep-deprived. The veteran’s speech is rapid and staccato; he displays hyperactive movements, with frequent scanning of the environment, terrified affect, and loss of contact with the immediate hospital reality.
An experienced female emergency psychiatrist quickly arrives but is unable to orient the patient or convince him to accept medical intervention. All questions regarding his current status are answered with phrases indicating the patient is re-experiencing combat in Iraq. His behavior is increasingly unpredictable and aggressive, leading the ED physician and psychiatrist to be concerned about the safety not only of the veteran but also of other patients and staff. All involved wish to avoid use of force if at all possible, certain this will retraumatize the patient and reinforce his dissociative state.
The ED physician, an older man, tells the psychiatrist that he is an Army veteran and a colonel in the Reserves....
(click below for complete story) http://www.psychiatrictimes.com/display/article/10168/1468071?verify=0 )
October 6, 2009
Psychiatric Times. Vol. 26 No. 10
CASE VIGNETTE
A 24-year-old veteran of Operation Iraqi Freedom (OIF) presents to the ED mid-morning on a weekday. While the veteran is waiting to be triaged, other patients alert staff that he appears to be talking to himself and pacing around the waiting room. A nurse tries to escort the veteran to an ED examination room. Multiple attempts by the ED staff and hospital police—several of whom are themselves OIF veterans—are unsuccessful in calming the patient or persuading him to enter a room.
The increased attention escalates the patient’s behavior and he begins to run around the ED. At one point he hides under instrument trays, yelling out “Incoming! We have to get them before they get us! The enemy is coming for us!” He then runs to another location, as if taking fire.
A quick general status evaluation shows a young man with several days’ growth of beard in jeans and T-shirt who looks sleep-deprived. The veteran’s speech is rapid and staccato; he displays hyperactive movements, with frequent scanning of the environment, terrified affect, and loss of contact with the immediate hospital reality.
An experienced female emergency psychiatrist quickly arrives but is unable to orient the patient or convince him to accept medical intervention. All questions regarding his current status are answered with phrases indicating the patient is re-experiencing combat in Iraq. His behavior is increasingly unpredictable and aggressive, leading the ED physician and psychiatrist to be concerned about the safety not only of the veteran but also of other patients and staff. All involved wish to avoid use of force if at all possible, certain this will retraumatize the patient and reinforce his dissociative state.
The ED physician, an older man, tells the psychiatrist that he is an Army veteran and a colonel in the Reserves....
(click below for complete story) http://www.psychiatrictimes.com/display/article/10168/1468071?verify=0 )
Monday, October 5, 2009
Urgent: Veterans' Healthcare Threatened
Published on Iraq and Afghanistan Veterans of America
By Michelle McCarthy
Created October 5 , 2009
This could be one of the most important phone calls you make this year.
Last week, the Senate failed to pass the VA budget, and six million veterans who rely on the VA for healthcare are paying the price. All passing the budget takes is one vote - the Senate just hasn't gotten around to it.
Now, VA hospitals and clinics nationwide can't plan for critical staffing and equipment needs, leading to longer waits for appointments, and rationed care. This is completely unacceptable.
Take action by calling your Senators now. Tell them to pass the VA budget, so that veterans get the care they deserve. Click here to place your call - our online tool makes it easy. [1]
The VA budget has been late an astounding 20 times in the last 23 years. And every year we've had to fight to get it passed. But your phone call could change that forever. This year's budget includes a provision that will fund the VA a full year in advance. Advance funding the VA is IAVA's top legislative goal for 2009, and it means veterans' healthcare will never be rationed again.
So please place a call to your Senators now and make sure that the VA is fully funded this year, and for years to come. [1]
The only budget that Congress passed on time last week is the one that pays their salaries. Veterans shouldn't have to wait while Congress gets paid. Help us change that today [1].
Thank you for making your voice heard.
[1] http://call.iava.org/16/vabudgetcall
By Michelle McCarthy
Created October 5 , 2009
This could be one of the most important phone calls you make this year.
Last week, the Senate failed to pass the VA budget, and six million veterans who rely on the VA for healthcare are paying the price. All passing the budget takes is one vote - the Senate just hasn't gotten around to it.
Now, VA hospitals and clinics nationwide can't plan for critical staffing and equipment needs, leading to longer waits for appointments, and rationed care. This is completely unacceptable.
Take action by calling your Senators now. Tell them to pass the VA budget, so that veterans get the care they deserve. Click here to place your call - our online tool makes it easy. [1]
The VA budget has been late an astounding 20 times in the last 23 years. And every year we've had to fight to get it passed. But your phone call could change that forever. This year's budget includes a provision that will fund the VA a full year in advance. Advance funding the VA is IAVA's top legislative goal for 2009, and it means veterans' healthcare will never be rationed again.
So please place a call to your Senators now and make sure that the VA is fully funded this year, and for years to come. [1]
The only budget that Congress passed on time last week is the one that pays their salaries. Veterans shouldn't have to wait while Congress gets paid. Help us change that today [1].
Thank you for making your voice heard.
[1] http://call.iava.org/16/vabudgetcall
More colleges develop classes on how to treat war veterans
By Gregg Zoroya
USA TODAY
October 4, 2009
Universities are creating classes to train students in how to treat combat veterans and their families suffering from war-related mental health problems.
As psychologically wounded troops return from the wars in Iraq and Afghanistan, the initiatives range from workshops to semester-long graduate courses, such as one on military culture next year at the University of Washington-Tacoma. The University of Southern California is starting a master's program in which students will interact with holographic images of troops in distress
"I think across the nation, a lot of schools of social work have concluded that we need to do something," says Jose Coll, director of USC's military social work program, which offers a degree that emphasizes treating veterans.
In addition to treatment methods, the classes teach military culture, the combat experience and what military families endure. That's a way of life that's mysterious to many new behavioral health students, educators say.
"This is sort of cultural awareness education," says James Martin, a retired Army colonel and Bryn Mawr College professor who has worked on several programs.
(click here for complete story)
http://www.usatoday.com/news/military/2009-10-04-ptsd-schools_N.htm
USA TODAY
October 4, 2009
Universities are creating classes to train students in how to treat combat veterans and their families suffering from war-related mental health problems.
As psychologically wounded troops return from the wars in Iraq and Afghanistan, the initiatives range from workshops to semester-long graduate courses, such as one on military culture next year at the University of Washington-Tacoma. The University of Southern California is starting a master's program in which students will interact with holographic images of troops in distress
"I think across the nation, a lot of schools of social work have concluded that we need to do something," says Jose Coll, director of USC's military social work program, which offers a degree that emphasizes treating veterans.
In addition to treatment methods, the classes teach military culture, the combat experience and what military families endure. That's a way of life that's mysterious to many new behavioral health students, educators say.
"This is sort of cultural awareness education," says James Martin, a retired Army colonel and Bryn Mawr College professor who has worked on several programs.
(click here for complete story)
http://www.usatoday.com/news/military/2009-10-04-ptsd-schools_N.htm
Subscribe to:
Comments (Atom)
"Grandpa Pat & Kain"
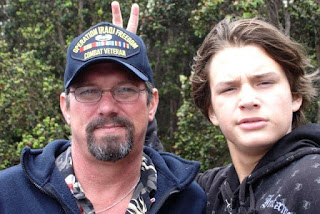
"Kain-man" the jokester....
Pat Lamoureux - Iraq 2003

"Pat is an extraordinary, thoughtful, kind and generous man...not to mention a wonderful friend, in which one could always count upon to be there when in need." (words of a long time friend)
Pat's Family

Mica & Heather, grandson Kain